The seasons are changing and the corona-virus is still here. In many parts of the world, a second wave has started. How can we stay safe and healthy during the coming fall and winter? Do we need a second lockdown? Not, if we take the right measures – and – importantly – if all participate.
Let’s start again with the basics. SARS-CoV-2 can be transmitted via surfaces, by direct spray processes such as coughing and large speaking droplets, and by aerosols that accumulate in the air. Individual safety measures matching these transmission routes include washing hands, keeping distance and wearing masks. Public authorities support this by mandating distancing and wearing masks in many places, and by tracing the contacts of infected people. Not all measures seem to work. Is this true – or did the measures ignore important scientific facts? What can we (and the authorities) do to make them work? Let’s look at the strategies. They can be distinguished between those where individuals need to take action, and others where the lead is with companies and governments. In this first part, I look at what an individual can do.
Individual measures
Get tested (or isolate yourself) if you have symptoms: You can spread the disease if you are infected. Not all have symptoms, but if you do, you should get tested and isolate yourself until the results are known. Actually, trying not to share a „normal“ flu or cough is also a good idea!
Wash hands: While it is easy to not shake hands, not touching door-handles, interactive displays or hand-rails in buses (to give just a few examples) is not really an option. Thus, washing hands is an important and effective measure. Yet it has a downside: if you wash your hands too often with soap and aggressive chemicals, you risk skin problems such as eczema. So you need to take good care of your hands to prevent dermatological problems. For example, use alcohol-based hand sanitizers with moisturizers rather than soap if you don’t have to remove actual dirt.
Wear a mask: The purpose of wearing masks it twofold. First, you prevent spray-transfer of viruses, and second you prevent inhalation (and build-up) of airborne viruses. Every person releases droplets of spit and lung liquid, more when talking, most when talking loudly, singing, or shouting. The larger sprayed droplets typically don’t travel far and rapidly fall to the ground. But indoors, the smaller micro-droplets can accumulate over time. The levels in a small and ill-ventilated room can quickly reach high levels when the infected person is a super-spreader talking a lot (see my previous blog, those with high viral load can become super-emitters). Worst is to be in the near-field of such a person. Hygiene masks reduce the emissions of all aerosol sizes, not just large droplets (see above) but also small micro-droplets. They also provide some protection, though not sufficient if you are in extrem situations such as a medical staff attending COVID-19 patients.
Keep distance: It is a good idea to keep distance, especially indoors, also when wearing a mask. You avoid not just sprayed droplets, but you are also outside the „near-field“ of the person, the zone from where exhaled aerosols are mixed into the general room air.
Ventilate shared spaces: Aerosols carrying the virus can stay airborne for long time. By replacing or cleaning the air, you can reduce the viral load. But be aware that in small rooms, you would need a storm to be safe without mask, if a super-emitter is in the room with you for a prolonged time. So while ventilation and air cleaning devices can help in small rooms, they do not replace the need to wear masks.
Avoid unnecessary in-person contacts. Staying put to yourself and your family is effective but it can be a lonely thing if you confuse it with locking yourself with your family in a fallout shelter. It rather means that you work from home when possible, try to limit the number of contacts, and postpone meeting loose acquaintances and strangers (unless there is an urgent need) to a time after the pandemic.
Don’t cheat. Don’t try to find ways to circumvent safety measures. For example masks work only if they cover nose and mouth, the edges have to touch the skin, and the straps have to be tight. But there are (too many) people in public places who see masks as a burden and find reasons to not wear them (correctly). Some will bring an (empty) cup of coffee or a beer can to pretend they are drinking, which is (at least in Switzerland, unfortunately) an accepted excuse for not wearing a mask. By not following safety measures, you put yourself and others at risk.
Shop wisely: The pandemic has shown us the fragility of our supply chains if only a few countries produces all the goods. You can help! The most powerful support for local producers comes from your wallet. Buy locally produced masks and safety equipment. Ask your boss to buy local products. Ask your government and policy makers to support local production. Demand mandatory declaration of the production place in (online) shops. Expose companies that brag about the „local design“ of safety equipment if it is made far away and thus not available in the next global lockdown.
So how effective are these safety measures?
How effective are these different measures? Which works best? To compare masks, room size and ventilation (or air cleaning), I use the formula we developed for our JAMA Network Open article.
- In each case, I calculate the inhaled „virus copies“, the number of virus-RNA-copies we expect to detect in the air (See box below about the infection risk of virus-RNA-copies). I do not consider direct spray transfer of large droplets or hand-to-mouth transfer.
- As a baseline, I first calculate your inhaled dose when you spend one hour with a mostly quiet Super-Emitter without symptoms in a room with a volume of 50 m3 and an air exchange rate of 1 per hour.
- I then calculate your inhaled dose if both, the emitter and you wear a good fitting hygiene (surgical) mask.
- Finally I calculate what volume or ventilation rate change is needed to have the same effectiveness as wearing a mask. The other factors are unchanged to see the stand-alone effect of volume or ventilation change.
The following figure illustrates the result of this modelling:
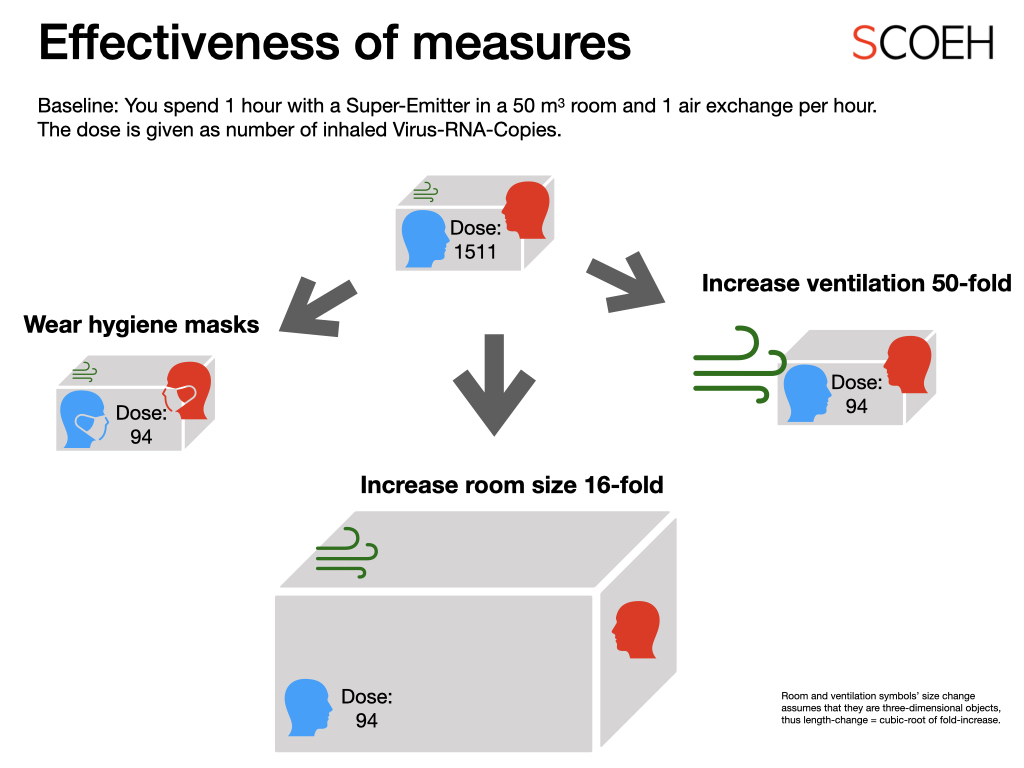
Figure: Approaches to reach the same efficiency as wearing a hygiene mask when spending one hour in a room with a mostly quiet super-emitter.
First, wearing well-fitting hygiene masks is indeed effective. In comparison, we would need to increase the room size by a factor of 16 to to 800 m3 (this means you meet in a big hall!), or increase the ventilation rate to 50 air exchanges per hour (this means you create an indoor-storm!). In reality, the room size would likely need to be even larger because usually the ventilation rate is defined as a function of people in the room. Also, making a 50-fold air exchange is rarely possible because you would need enormous ventilation ducts, it would create an infernal noise, and the wind speed would be very uncomfortable.
So, masks are by far the most efficient way to keep airborne virus levels low. Given that you rarely will be able to convince your boss to let you work in a huge hall, and that ventilating at 50 air exchanges is only possible in paper free offices (let alone the energy it would require and the loss of comfort), we see that increasing ventilation and room size are rarely suitable as stand-alone solutions.
However, increasing ventilation and room size can be supporting actions. If you work with others in a very small office with bad ventilation and you all need to talk a lot (which increases aerosol emissions), masks alone will not be sufficient if one of you is a very high emitter. Here, better ventilation and moving to a larger office (or moving the often-speakers to a single office) clearly can help. We also need to keep these measures in mind when looking at strategies that companies and governments can take (which is the topic of a future blog).
What are Virus-RNA-Copies? Can you define a safety limit?
After a virus pirated a cell, it forces it to produce new viruses. However, this virus production is not precise. Not all viruses get correctly assembled and only a fraction of these „virus copies“ is infectious in cell tests. These cell tests often provide a unit called PFU = Plaque Forming Units. PFUs are the number of visible spots on a cell culture dish, which result from infected cells infecting those around them. Even if a few infectious viruses get into the body, this is often not enough to make a healthy person sick. For many viruses a few hundred PFU are needed to be sure to infect the target organism. The PFU-number causing airborne infections in humans is not yet know for SARS-CoV-2 (the virus causing COVID-19), but some virologists guess it is in the range of a few dozen to hundred PFU (i.e. similar as for the Coronavirus that caused SARS). However, we want to avoid infections. So a more cautious estimate is that you are probably safe if your dose is below a few hundred „virus copies“, which corresponds to a few PFU. Now, for an „at-risk“ person, it may be safer to not inhale any PFUs at all. At a dose below 100 virus-copies, there is already a good chance to have no or only one or two PFU inhaled. Clearly more studies are needed to confirm this guessing.
