The Corona-Virus can be transmitted through three different routes: via direct hand to mucosa contact (wash your hands regularly!), by large „sprayed“ droplets (keep distance), and by aerosolised microdroplets (wear a mask).
We recently published a model to estimate viral aerosol emissions from simulated individuals with asymptomatic to moderate COVID-19 (see footnote). In this article, we simulated the two extreme sides of virus-loaded aerosol emissions by humans: regular breathing and coughing frequently. Already simple breathing resulted for some individuals in emissions high enough to infect others. In-between these two extremes lie the emissions from speaking and exercising. Speaking softly will increase the aerosol volume emissions by a factor of about ten, speaking loudly and singing increases this further. Also exercising can easily double to quadruple the emissions.
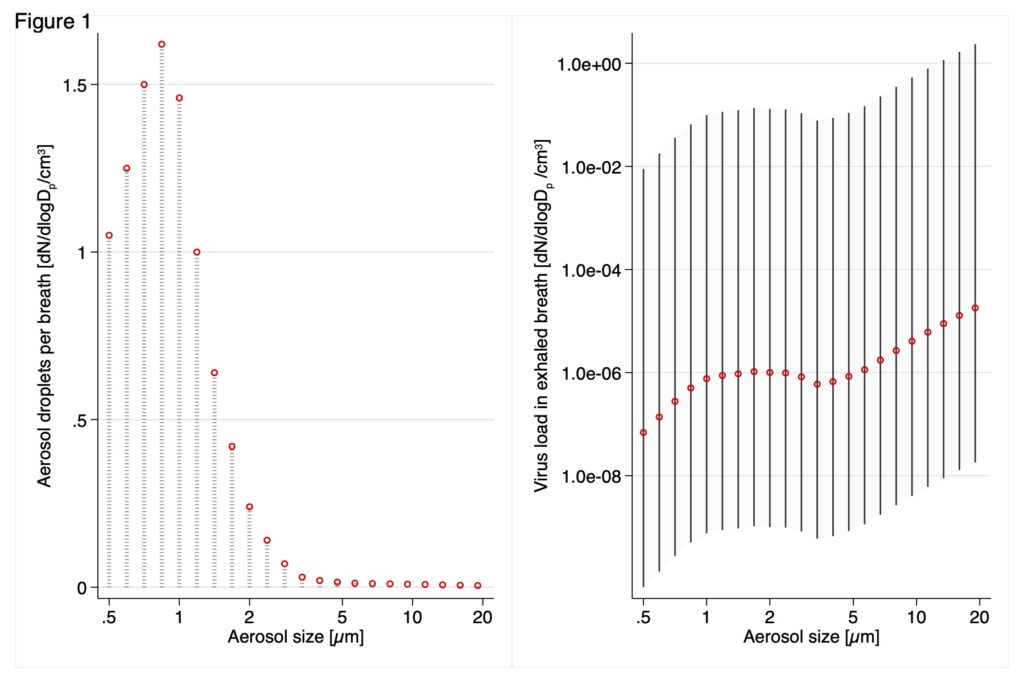
Figure: Size Distribution of Exhaled Microdroplets and Resulting Viral Emissions During Regular Breathing. Left panel: The typical exhaled microdroplet concentration used as input for the simulation. Right panel: The modeled viral emission per breath for typical (orange), high, and low (whiskers) emitters. dN/dlogDp/cm3 is the number concentration normalized by the aerosol size-bin width.
The most critical determinant for high viral emissions in our model was the viral load in the lung lining liquid. This ranges from a few hundred virus copies per millilitre to 10 billion copies/ml. Only those people having a very high viral load emitted sufficient virus to be a problem for airborne transmission.
Does this mean that all this talk about aerosol transmission is exaggerated? No! To the contrary! Rare events lull us into a false safety. Think what airborne transmission implies: If you happen to be for more than a few minutes in the same room as a super-emitter, you are likely to get infected. And so is everybody else in that room. But our model also suggests that aerosol super-emission of viruses is a rare phenomenon. You can have many encounters with infected people and never have a problem. So you may think that you are safe.
Take the example of singing in a choir. Did you realise that there was only a handful super-spreading events world-wide for this scenario? Compare this to the many choral rehearsals that went ahead in the early time of the crisis! Our model aligns very well with this observation that super-spreading events are not frequent.
Super-spreading is rare but a big public health problem
Your chances to meet a super-spreader in Switzerland are probably small. But the risk coming from these super-spreaders has to be seen from a public health perspective. You can illustrate this well by looking at travelling by trains.
- Assume we have one infected asymptomatic person per train
- Assume one permille (1/1000) of these infected people is a super-spreader.
- Consider that there are over 9’000 passenger trains circulating on Swiss rails per day.
This (probably too simple) model implies that we have each day 9 train coaches where people spend time with a person who can infect them via aerosols! Isn’t it good that in Switzerland, wearing masks in public transport has become mandatory?
Ventilation reduces the risk – but measuring CO2 is not giving the information we need
Recently, CO2-measurements were proposed to assess whether a room was sufficiently well ventilated. On Swiss TV, some ventilation experts suggested that below a limit of 1000 ppm CO2, people were safe from the virus. While keeping CO2-levels low is useful to reduce the risk of sick building syndrome, CO2 is not a good measure to assess the virus load. The CO2-level tells you about how many people you have in the room. But we are worried about the emissions of one super-spreader!
Let me explain this with a simple example:
- I take a class room of 10m x 10m x 3m (=300 m3).
- I assume a high ventilation rate of 5 air exchanges per hour (= 25 m3 per minute!).
- I put into this room a super-emitter talking 10% of the time loudly (= 10x increased emissions compared to breathing normally).
- I add people in the room.
- I wait 60 minutes.
- I calculate the virus concentration and the CO2-levels after 60 minutes (same model, of 35k ppm CO2 in exhaled air at 7.5 liters/min per person).
Viral airborne concentration in this room: 1830 virus copies/m3
CO2 concentration with 2 people in this room: 420 ppm
CO2 concentration with 10 people in this room: 500 ppm
CO2 concentration with 25 people in this room: 660 ppm
CO2-concentration with 58 people in this room: 1000 ppm
Do you see the pattern? In this room, five air exchanges were sufficient to keep CO2 in a „healthy building“ range, even with many people in the room, but the virus level was always in the infections range! With few people in the room, we would feel very safe when looking at the CO2-levels. But attention, here, elevated CO2-levels only tell us that many people will get infected.
So what can you do?
- Fresh air: While ventilation alone is not a solution, it does help to reduce the virus concentration. So keep on ventilating!
- Wear a mask. Wearing a mask is a good way to reduce emissions. Make sure your mask has a good fit (no leakage on nose, cheeks, and chin). Also, get a mask with at least three layers of tissue, or a medical-grade surgical (hygiene) mask (if available in your country).
- Small social circle: Avoid situations where you have to spend a long time in the same room with many other people, especially if the other people change frequently.
Footnote: We developed this model in March. Initially, we had done the simulation for this blog but then figured it may be better to get it validated by scientific peer review. In late July, after a lengthy review, some corrections of the underlying math and several revisions to update the literature, it was published in JAMA Network Open on 27 July 2020.
