Imagine you are a pilot. Suddenly a flock of geese hits your flaps, your engine turns off and your plane goes into a steep dive. Will you just try to flatten the curve? No. You must simultaneously regain control over your trajectory, assess what systems still work, try to restart the engine and also think of and prepare for emergency landing options.
Most countries were not as well prepared for the virus as pilots are for a goose strikes. Few had detailed checklists (functional pandemic plans), emergency training and a leadership that took swift, decisive and elaborate actions. So what if your country is in a steep dive? Is it enough to just tell everybody to stay home until the virus is gone?
No. Crisis management is similar to a game of chess. You have to think several steps ahead, you have to re-asses the situation after each draw, and you may have to sacrifice a pawn to win the game. To be clear, I am not talking about sacrificing human lives, but about a continuous rational weighing of values as we do already when we limit the freedom of movement for the sake of preventing new infections. But this is not the only option.
Develop questions and scenarios to define research and to find new approaches
To identify what steps we can take now and later during the crisis, governments (and also companies and individuals at their own level) need to have an overview of all possible scenarios, even those you do not want to take. This will allow you to make a weighing of values and assess which options promises the best overall effects for the country and its people. For producing reliable, evidence-based scenarios we need facts about the disease, all imaginable protective and offensive strategies, how well they work and what effects they may have on economy and society compared to the baseline to „just lock up everybody“. To develop such scenarios, a few governments already started to set up expert panels that come from many different scientific disciplines. It is smart to consider also what we can learn for the next crisis and which tools we may want to keep in our quiver, as it is worthwhile to choose more expensive high-quality solutions if they are going to last.
It will be important to allow scenarios to question current beliefs and ideologies (e.g. the mantra of „wearing masks in public does not help“) as long as they are based on scientific facts. The scenarios need to be well-elaborated and address the different aspects of life and society. In some cases we may have to gather more facts, in others we have to find out how to implement the measures efficiently, or what needs to be done before we can do something.
Scenarios builders need to think of a wide range of research and development. While it is important to rapidly develop cures and vaccines, we also need research on non-medical approaches to gain some kind of „normality“ until we can get rid of the virus.
Here a few examples of questions that can help develop scenarios. Note that these questions are highly interlinked!
- We need much more fundamental information about the virus. We already know the virus can get airborne and it can be on very small particles. It can persists for many days on surfaces and not all biocidal agents are effective. What does this mean for safety measures in hospitals, infected homes and public spaces? At what levels do we have to consider direct transmission and resuspension of dust containing viruses as a route of infection? How can we confirm a space is safe to re-enter without protective gear? These questions also relate to the infectious dose of SARS-CoV-2, which is poorly understood. For testing the efficacy of many applied approaches, it would be very useful to have surrogate particles for testing that behave similar to the virus, also with regard to the stability in various environments so that wide-spread tests can be conducted without spreading the actual virus.
- We are very close to rapid tests to identify cured and healthy people. For example, antibody tests promise to soon allow cheap and rapid identification of people who had the virus. Also, some initial reports suggest that 3D-lasers and photo-acoustic scanners may help differentiating healthy people from non-symptomatic cases within a few seconds. Can we use such technologies to allow healthy or recovered people to resume work?
- How can we keep people safe and healthy in public buildings, transport systems, and shared workplaces? We can restart public life only once we have an answer to this question – or a cure or vaccine. Does it help when everybody wears a mask? What is necessary to effectively prevent contact contamination? Do we need mandatory hand-washing stations in public transport, shops and populated areas where people are frequently close together?
- Is there a way to allow opening low risk shops such as consumer good shops and workshops that do not require direct physical contact? After all, people still need clothes, shoes, repairs etc. and not all of this is easily acquired by online-shopping, for example seedlings for your garden, or finding clothes when your body is not having standard measures.
- Under which conditions can we allow high-risk businesses where direct physical contact is required such as hairdressers, manicure or massages? Is it enough to have everybody wear hygiene masks, wash hands, and disinfect surfaces, or should the staff wear suits like they do in South Korean ICUs?
- How can we prepare schools for re-opening? Do we have to wait until the last case is gone or are there ways to do this sooner? Should’t we start now to develop and test technical and organisational measures for schools? Many health and safety measures known to work for toxic chemicals could be considered as a way to allow resuming at least frontal teaching classes, but the technical implementation and the usability for kids has to be carefully tested. This testing can quickly take months, so it seems best to look soon into these questions.
- Do we know enough about food safety? How can we prepare uncooked food such as salads to be safe in case it was touched by somebody infected? What consignments do we give to canteen and take-away operators, but also the entire food industry? Is it enough to just wash hands, or should they all wear hygiene masks?
- Spring is coming and so are pollen. How do we keep asthmatics out of the emergency rooms? What symptoms warrant that a hay fever sufferer calls the doctor? Is all the medication still save to be taken?
- How can we include the public in reacting to new infections? Should we rethink our approach to privacy during the time of crisis and publish refined geographic information such as the living and working town of cases as well as their public transport commute route until they were isolated? What are the ethical and legal implications? Under what circumstances could this be societally acceptable?
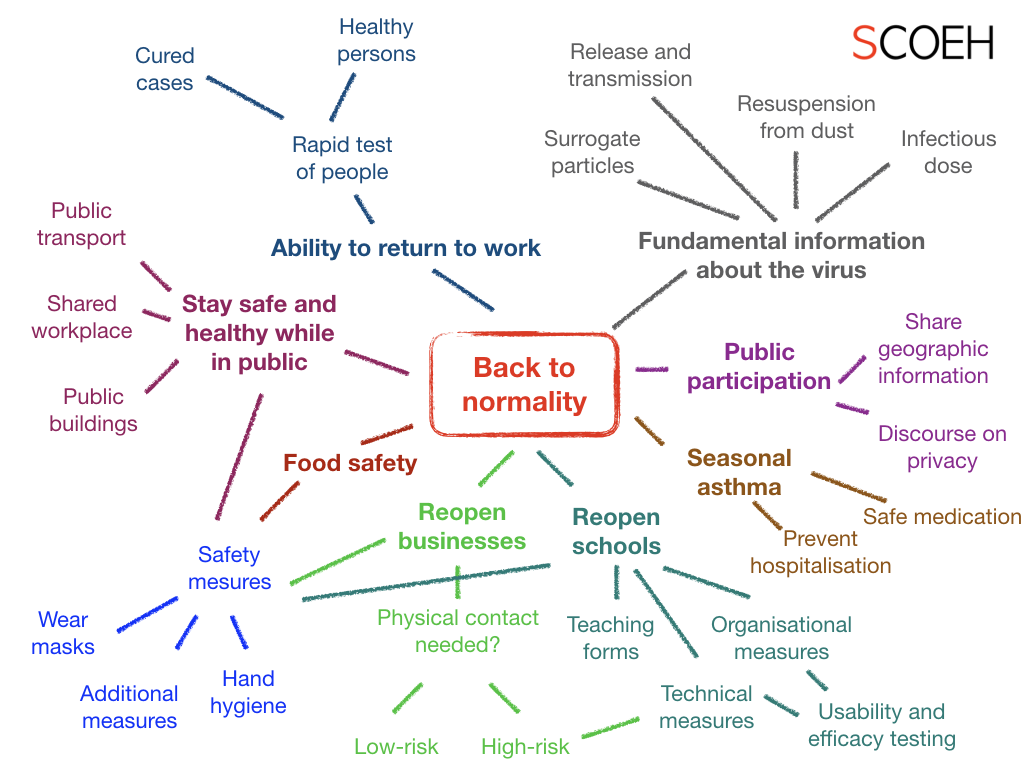
An incomplete mindmap to illustrate elements we need to address to get back to normality.
This list can continue for a long time, see also questions asked earlier in my blog surrounding sampling strategies, washing hands, using masks, sharing data etc. Answering the above and more questions will require the collaboration of researchers and practitioners from many disciplines such as virologists, epidemiologists, mathematicians and statisticians, biologists, occupational health and safety specialists, engineers and mechanics, ergonomists behavioural and usability experts, sociologists, psychologists, economists, and legal and governance experts. There are also many highly applied aspects so it will be important to reach out to practitioners outside the academic field, and to structure the research funding tools and rules accordingly.
.
